Animal experimentation: 3D for 3R
More than 600,000 animals a year are used in experiments in Switzerland alone. Despite tougher animal protection regulations, the number remains high due to ever stricter patient protection requirements: the safety of new drugs must first be proven in animal tests. In order to reduce the number of animal experiments, HLS researchers are working on alternatives such as cellular 3D test systems designed to emulate organs and their function. The HLS team have now established the efficacy of their tests for kidney cells and for disease-altered liver tissue.
A cell is clearly very different from a whole organ. However cell cultures can be used as models for re- search into cell division, metabolic processes or signal transmission, as well as for testing the effects and risks of new drugs. However, conventional cell cultures are less efficient at showing the influence of structures and environmental interaction. Hence the need for animal experiments. Or perhaps not. According to toxicologist Laura Suter-Dick from the Institute of Chemistry and Bioanalytics, a large number of animal experiments may soon be redundant, replaced by growing tube-shaped 3D kidney cells which imitate the structure of a real kidney. “If you can already see in an organ-like cell culture that an active substance damages the cells, you do not need an animal experiment anymore”, Suter-Dick says. That goal is reached using Organo- PlateTM cell culture plates to replicate the tiny tubes in the kidney: a gel is introduced along several small parallel channels on the cell culture plate, forming guide tubes on the inner walls of which kidney cells are grown. “This new biochip technology has enabled us to create kidney cells in the form of small tubes, like in a real, healthy kidney, which we can use for tests”, says Suter-Dick. The kidney has an important detoxification function in the body, filtering harmful substances and blood metabolism end products and transferring them to the urine. Due to this filter function, the kidney is heavily exposed to the degradation products of drugs which can permanently damage the small tubes in the kidney. Hence why pharmaceutical companies must test every new drug for its effect on the kidneys and their filter function. Suter-Dick: “There are still areas in toxicology or in pharmacology where animal experiments have to be done however. They cannot be re- placed because the regulatory authorities put patient safety first.”
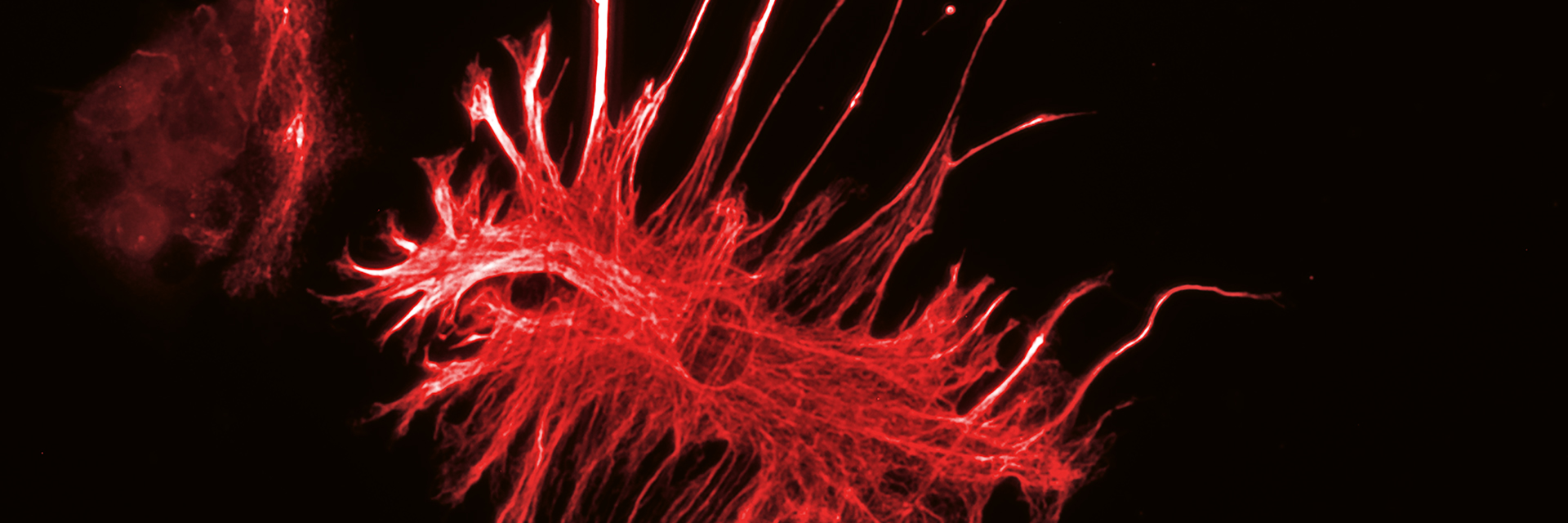
Suter-Dick bases her research on the 3R principle: replace, reduce and refine. The aim of this 1959 guideline is the responsible treatment of lab animals as well as the reduction and replacement of animal experiments. Although animal experiments are subject to very strict regulations in Switzerland and are only approved after examination by cantonal animal experiment commissions, they remain ethically controversial. A majority of the animals are used to investigate the toxicity of new active ingredients in healthy organisms, as required by law before it allows the use of a new drug in humans. About 2% of drugs at the pre-clinical stage and 19% of those in a Phase III trial never get to the market because they cause kidney damage. Failure at such a late development stage means not only a high cost to the pharmaceutical companies but also a senseless use of test animals during the drug development phase. Since most drug-induced kidney damage affects the proximal tubules, Suter-Dick is focusing on these complex structures: “The proximal renal tubule cannot be mimicked in normal cell cultures as it consists of several cell types that form a tubular structure and perform different tasks.” Normal kidney cells have a transport function that allows them to import or export drugs and other substances. Many conventional cell cultures cannot emulate this transport function and can thus seldom be used to test for renal toxicity, leaving no alternative to healthy test animals.
Suter-Dick’s work, in collaboration with two research partners from the Netherlands (Radboud University and Mimetas), is funded by the British National Centre for the Replacement, Refinement and Reduction of Animals in Research (NC3Rs). Together they have investigated the transport and barrier functions of kidney cells using 3D techniques. Damage to renal cells from substances such as immunosuppressive agent cyclosporin A or virostatic agent tenofovir can be demonstrated by elevated biomarkers in patients’ blood or urine. The same biomarkers, usually monitored in the lab, have been tested by Suter-Dick in 3D cell cultures, show- ing their efficacy with a high throughput system which can test many substances in parallel, saving both time and money.
In another project, rather than a healthy, normal cell system the toxicologist has developed a liver disease model in the petri dish. The aim is to avoid rats and mice being exposed to a particularly hard group of experiments: they are bred as mutants with specific diseases or the disease is chemically induced to obtain very accurate understanding of clinically relevant diseases. Such “models” are necessary to see the effect of new drugs on the exact symptoms for which they have been developed. However, since many metabolic processes
work differently in animals from humans, the significance of those experiments can be limited. There is still no effective animal model that realistically replicates common liver fibrosis — a late stage of chronic liver disease. Despite that, thousands of rats and mice used as test animals for liver fibrosis suffer every year. These animal experiments last a long time and add significantly to the pharmaceutical companies’ high costs of developing new active ingredients. The firms are thus stepping up the search for alternative ways to test liver fibrosis drugs in vitro. Cell culture experiments make it relatively easy to work with human tissue, increasing the relevance of the findings for patients. However, normal cell cultures cannot emulate the disease pattern of liver fibrosis, since it produces three types of cells which must be activated one after the other in order to form its fibrous scar-like tissue. A further complication is that liver fibrosis can only be induced by the constant effect of a harmful substance, which takes more than two weeks in the laboratory.
In a CTI project, Suter-Dick in collaboration with the Swiss company InSphero, has developed a 0.3mm diameter spherical cell culture model which contains all three cell types needed for the forma- tion of liver fibrosis. “The hardest thing was to activate and combine the different cell types so that they function together correctly”, the scientist says. Her experiments have provided the first evidence that the 3D liver fibrosis model works and can be used by firms and other researchers. The next step will show whether it is possible to prevent the activation of the liver cells and therefore to develop potential remedies for fibrosis.
- Cell cultures with primary cells and cell lines
- organ-on-a-chip technology
- microfluid systems
- InSphero hanging drop technology
- viability assays
- impedance measurements
- gene expression analysis
- cell staining (histology)
- immunofluorescence, confocal microscopy
- Cell culture accessories, including microfluidic systems (U-cup, Minucells, own apparatus) and bioprinting
- 3D-cultures: organoplates (mimetas), micro-tissue (InSphero), Transwell systems, microencapsulated alginate spheres
- Analytical methods: western blot, ELISA, receptor interaction (Flex station), qPCR (Corbett rotor)
- Functional tests: cell respiration (seahorse) and cell growth (xCelligence) microscopy, including confocal microscopes
- NC3Rs, CTI
- Mimetas B.V. Leiden, Netherlands
- Radboud University, Netherlands
- InSphero AG Schlieren
- SCAHT Basel