Improving wound healing after C-sections
Reto Wildhaber’s team has developed a visualisation technology to better illuminate corrective surgery after caesarian sections
In Switzerland, 32% of babies are delivered by caesarean section. While hospitals are working to reduce the number of procedures that are not medically necessary, Switzerland’s rate remains one of the highest in Europe.
Caesarean sections pose several risks to the mother, one of which is poor healing of the uterine scar. Unknown tissue factors can lead to hampered wound healing and gaps in the anterior uterine wall. These gaps, also called niches, weaken the uterus in a subsequent pregnancy. It can take 1-2 years for women to observe pain and other complications from improper wound healing, which might require follow-up corrective surgery. Chronic pain and multiple surgical interventions can prevent women from performing childcare duties and returning to the workforce, and can considerably reduce their quality of life. If the niche breaks during a subsequent pregnancy, there are significant risks for both mother and baby.
Surgeons at the University Hospital Zürich approached Prof. Dr. Reto Wildhaber with the idea of integrating a light source into a uterine manipulator, a tool used during gynaecological surgery. Current laparoscopic tools and camera systems for imaging the uterus during corrective surgery emit light only outside the uterus, and provide an unclear view of different layers of tissue inside the uterus.
Wildhaber, who specialises in signal analysis and digital biomarkers, came up with the idea to use a pulsing light that is inserted into the uterus through the vagina and cervix. He supported the development of the first prototype while working at the Berner Fachhochschule (BFH). In 2021 he joined the Institute for Medical Engineering and Medical Informatics and continued to work on the project in collaboration with BFH, with whom a joint patent has now been filed.
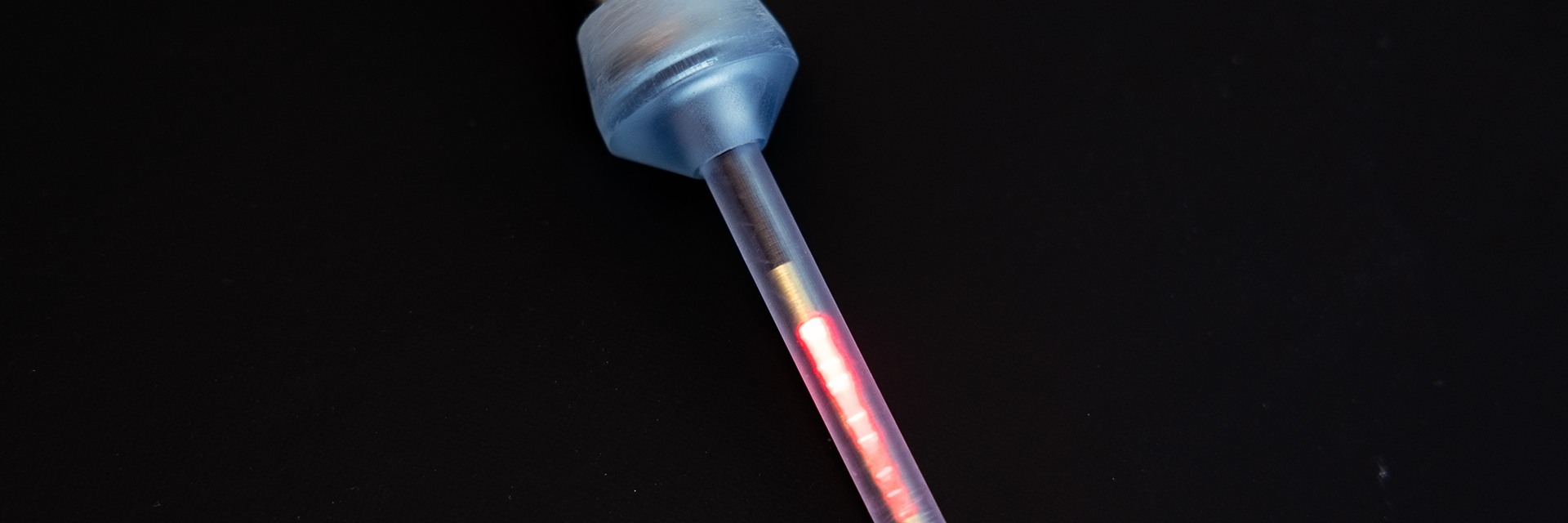
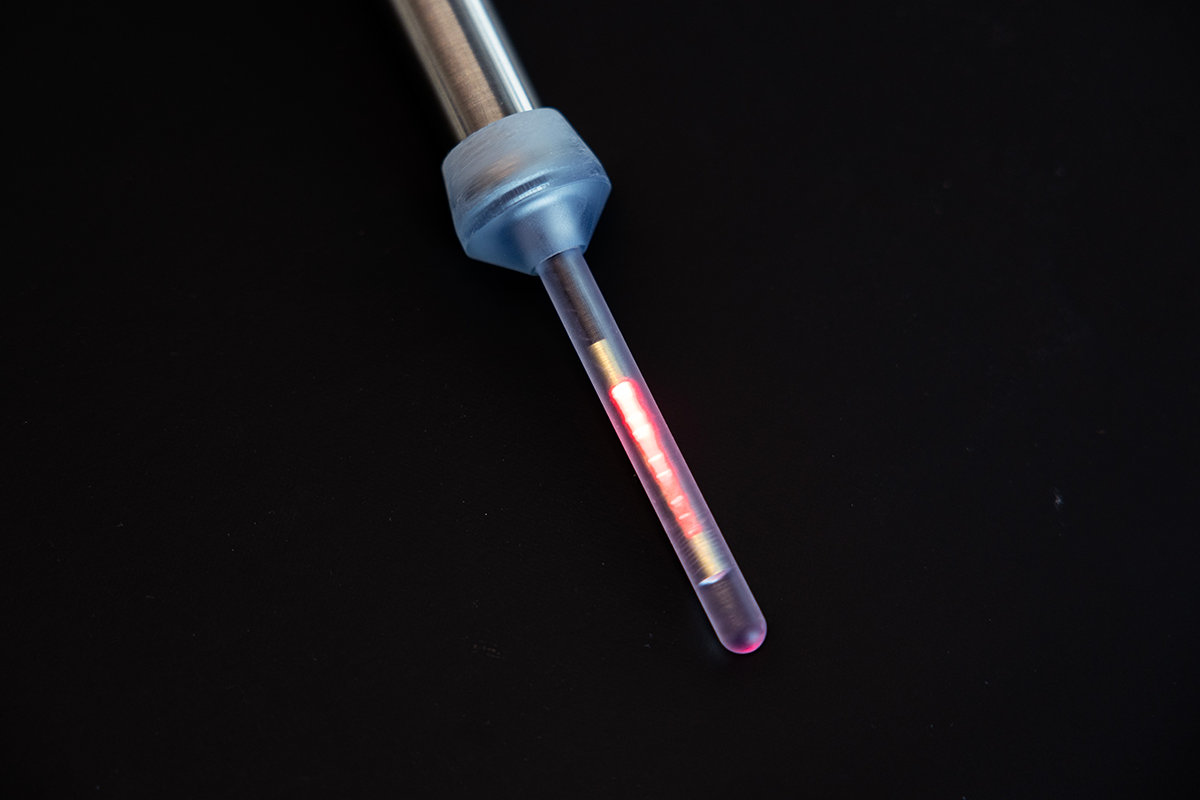
First, Wildhaber’s team tackled the physical challenges of refining the prototype. They selected the material and process to produce the instrument tip where the pulsing red LED light source is housed: 3D printed biocompatible polymethyl methacrylate. The tips were subjected to mechanical force testing to ensure they can bend during surgery without snapping.
To facilitate sterilisation, the instrument can be disassembled into components and laid flat in an autoclave. The conical design of one component acts as a ‘plug’ for the cervix, stabilizing the instru-ment and preventing gas injected into the abdomen during surgery from escaping the uterus. To keep the tip of the instrument cool and prevent damage to uterine cell tissue, fibre optic cables are used to transmit light from the pulsing red LEDs into the uterus.
The team then put mathematics into action, developing a digital enhancement equation that exploits the difference between the pulsing interior light emitted by the prototype, and the exterior light emitted by laparoscopic tools, to create an image overlay on the surgical monitoring screen. The 2D augmented reality will help guide surgeons by displaying the boundary of different tissues in the uterus and the location of the surgical tool. It will enable them to see the niche and precisely remove scar tissue.
Overall, the instrument provides an intrauterine light source that allows direct localisation of the niche while stabilizing the uterus, and is compatible with the DaVinci robot that assists the corrective surgery. The small computer required to perform the digital enhancement equations and the screen that displays the 2D visualisation can be easily integrated into existing laparoscopic set-ups.
The visualisation technology underwent a proof-of-concept pilot study in Wildhaber’s lab in the summer of 2024, which will be followed by clinical studies at the Department of Gynecology at the University Hospital Zürich after approval by Swissmedic and the local ethics authorities.
“We believe that women with lower abdominal symptoms and women with a niche that wish to conceive a second child will profit from the new device” says Prof. Dr. med. Cornelia Betschart Meier. “We are looking forward to applying the so-called scar light device in a first clinical trial. It will enhance the surgical technique and we expect it will yield a good outcome for mothers and children.”
“This device has the potential to simplify a medically necessary procedure, and make it safer and more reliable, thanks to today’s technology” says Wildhaber. If clinical tests are successful, a spin-off company at USZ could be formed, or the technology could be licenced to a surgical or imaging instruments firm in order to bring it to the market.
Key facts | |
|---|---|
Patients / Target Groups: | Gynaecological health |
Partners: | University Hospital Zürich, Fachhochschule Bern |
Financing: | Innosuisse 101.964 IP-LS |