Navigating the brain
Céline Vergne has developed an intelligent electromagnetic navigation system for precise implantation of deep brain stimulation electrodes
The success of deep brain stimulation (DBS) depends on precision, both in positioning the electrodes and stimulating specific brain regions. Currently, pre-operative imaging and stereotactic techniques are the gold standard for the insertion of DBS electrodes into the brain, but they do not offer tracking during surgery.
Céline Vergne, who is completing a PhD at the Institute for Medical Engineering and Medical Informatics with a joint enrolment at the Universities of Basel and Strasbourg, has developed an electromagnetic navigation system aiming at the precise tracking of electrodes during their implantation. “The chip integrated into the stimulation device, coupled with our visualisation system, will allow surgeons to see the angle and position of the DBS electrode” says Vergne.
She first integrated a tiny magnetometer into the electrode. Less than 1 mm across, the magnetic sensor can be detected by generating low magnetic fields and using a tracking algorithm to determine its position. Prof. Dr. Joris Pascal’s team contributed to the sensor’s development, while Prof. Dr. Simone Hemm’s team was responsible for the system set-up and testing in the surgical environment. In collaboration with the University of Strasbourg, Vergne is investigating machine learning algorithms to optimise the sensor’s tracking performance.
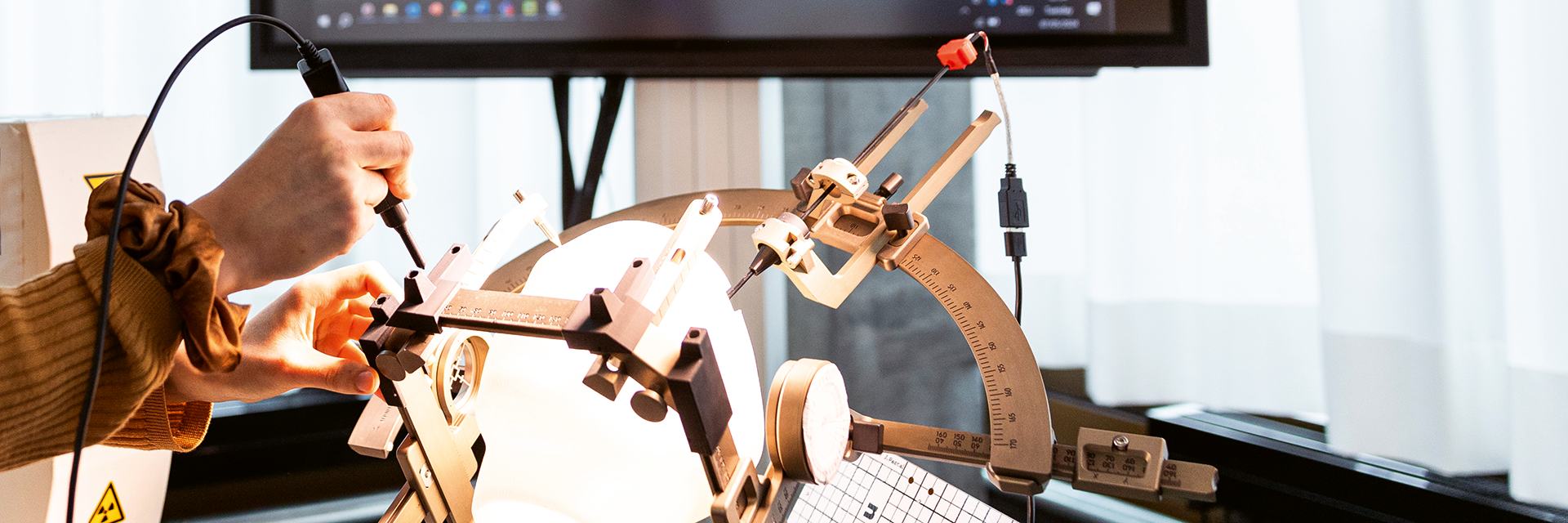
Vergne then set out to ensure the compatibility of her prototype with the surgical environment. In the operating lab at the FHNW School of Life Sciences in Muttenz, she recreated a DBS surgical set-up using a head phantom inside a stereotactic headset. For the electromagnetic navigation system, called ManaDBS, she added a system control unit, a magnetic field generator and a sensor interface unit connected to the DBS lead.
Electromagnetic perturbations from the magnetic field can throw off tracking. To address this, Vergne applied a new tracking principle to limit electromagnetic disturbances and ensure correct tracking of the electrode.
Implantation trials on an eggplant simulating brain tissue were performed in a recreated DBS surgical setup. This gave an initial idea of the sensor’s performance. The final step before transfer to the clinical environment is user-friendly software to visualise tracking in the operating room.
The system will then be tested at the University Hospital Basel during a surgical dress rehearsal. This environment can simulate the compatibility of the technology with the unique DBS operating theatre, helping translate the prototype to the clinic.
If successful, a team of neurosurgeons at the University of Basel will test the technology in patients. Ultimately, the system may go through medical device approvals, led by a producer of neurosurgical or navigation instruments.
“It’s very exciting to have three fields coming together in this project: electronics, computer science and neuroscience” says Vergne. “This multidisciplinary approach and collaboration with partners are driving innovation forward.”
“This electromagnetic navigation system is a promising tool for the localisation of the DBS electrodes. We are hopeful that it will be integrated into the surgical procedure and bring advantages for both patients and medical teams” says Dr. Ethan Taub, Neurosurgeon at the University Hospital Basel and external expert of the project.
Key facts | |
|---|---|
Patients / Target Groups: | Parkinson’s disease, essential tremor, dystonia, epilepsy, chronic pain |
Partners and PhD Co-Directors: | University of Basel: Prof. Dr. med. Raphael Guzman, Chairman, Department of Neurosurgery Université de Strasbourg: Prof. Dr. Morgan Madec, Simulation and electronics systems |
Financing: | SNSF 204448 |
Deep brain stimulation - Did you know?
In the late 1980s, a French breakthrough in neurosurgery, deep brain stimulation (DBS), opened new avenues for the treatment of movement disorders. DBS involves the implantation of electrodes and tiny neurostimulators in the brain. These devices send signals to specific targets in the motor regions, to help alleviate motor symptoms.
DBS was approved by the FDA in 1997 for the treatment of Parkison’s Disease and essential tremor. It is now also used to treat dystonia, some obsessive-compulsive disorders, epilepsy and chronic pain. It may be combined with taking medicines, or offer an alternative to them.