Testing brain medicines in the fast lane
New in vitro model of the blood-brain barrier helps pharma identify promising candidates
The need for brain therapeutics is great, and many pharmaceutical companies are developing drugs. To test these novel medicines, clinically relevant models that measure their ability to cross the blood-brain barrier are needed.
In vitro models are cells grown inside a special device that mimics how an organ, or part of it, functions. Prof. Dr. Laura Suter-Dick’s team at the Institute for Chemistry and Bioanalytics has deep expertise in developing liver models to test the safety of new medicines, while reducing and replacing the need to use animals for example.
Backed by this strong foundation in advanced in vitro models and new approach methodologies (NAMs), postdoctoral researcher Dr. Floriana Burgio from Suter-Dick’s cell biology group, in collaboration with scientists from UCB Pharma Belgium, set out to create a model of the blood-brain barrier using induced pluripotent stem cells (iPSC). These immature cells can be differentiated into any cell type, making them versatile for research.
The model implemented by Dr. Burgio features a single cell type: brain microvascular endothelial cells (BMEC) derived from iPSC. She grew the model in an OrganoPlate® (Mimetas) and conducted tests to confirm that it mimics barrier tightness. The model features a top channel with endothelial cells, a middle channel with extra-cellular matrix, and an empty bottom channel. Test molecules are perfused into the top channel; those that bind and pass are collected in the bottom channel. The system is compatible with automated fluid handling and allows the evaluation of 40 chips simultaneously.
“When tested in our BBB model, we showed that a molecule which binds to the transferrin receptor has an 11-fold increase in crossing the barrier compared to a control molecule that does not bind” says Burgio. “This established that our model exhibits functional transferrin receptor-mediated uptake and transcytosis.”
The project was conducted in collaboration with UCB Pharma Belgium, a leader in medicines for neurological, immune and rare diseases.
“The FHNW’s model of the BBB represents a great step forward towards testing the ability of potential drug candidates to enter the brain. In the end, such a model can improve preclinical testing of future medicines from both an efficacy but also a safety point of view” says Rainer Class, Associate Director of In vitro ADME, UCB Pharma.
“Not only did this project enable us to develop a model that UCB Pharma Belgium can use as part of their drug screening process; it also allowed the FHNW School of Life Sciences to break new ground in designing in vitro models with induced pluripotent stem cells, propelled by the latest microfluidic technologies” says group leader Prof. Dr. Laura Suter Dick.
Key facts | |
|---|---|
Partners: | UCB Pharma Belgium |
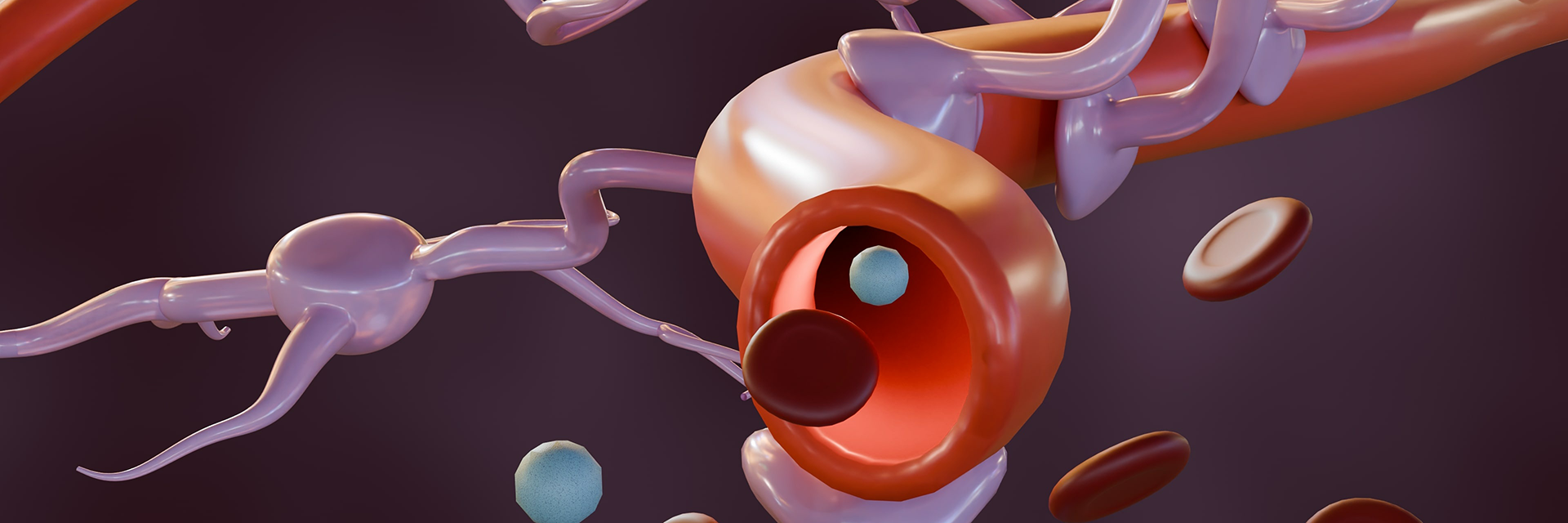
The blood-brain barrier: Did you know?
Our brain is protected by a layer of tightly woven endothelial cells that line the brain’s blood vessels, called the blood-brain barrier. These cells block foreign agents such as pathogens from entering our body’s command centre. At the same time, nutrients that the brain needs are allowed to pass, via a process called receptor-mediated transcytosis (RMT). Receptors on the surface of endothelial cells recognise and bind to nutrients, and carry them into the brain.
The barrier also prevents some therapeutics from reaching disease targets in the brain. Medicines that can successfully enter the brain include anesthetics, antidepressants and antipsychotics. A great need remains however for therapies to treat Alzheimer’s, ALS, Parkinson’s, brain cancers and more. Biologic drugs could offer hope, but strategies must be devised to sneak these large molecules past the barrier using RMT.