Using data to cope with tremors
HLS researchers have developed a method to make deep brain stimulation in Parkinson’s disease even more precise and thus more effective. Deep brain stimulation, in which an electrode is implanted in the patient’s brain, is a treatment for the symptoms of tremor and rigidity. The positioning of the electrode in the brain affects the level of improvement in the symptoms. The HLS’s data-supported imaging method can identify the best stimulation location more reliably, enabling better intervention planning.
Parkinson’s patients suffer from uncontrolled movement disorders such as tremors of the extremities and muscle stiffness, caused by dying nerve cells in the basal ganglia, an area of the midbrain that controls motor function. At present there is no cure. One treatment that can alleviate the symptoms of Parkinson’s disease is deep brain stimulation. It works in a similar way to cardiac pacemaker therapy, replacing the defective function of the damaged cells with electrical impulses transmitted from an electrode to an area in the brain a few millimetres in size. The challenge is to implant the electrode in exactly the right place in the brain. Imaging techniques such as magnetic resonance imaging (MRI) and computer tomography (CT) can help, but the images do not show exactly where stimulation is needed. Simone Hemm-Ode from the HLS Institute for Medical Engineering and Medical Informatics (IM2) and her team have developed ‘Improvement Maps’, a method for measuring symptom variations during deep brain stimulation and visualising the data obtained on CT and MRI images.
“Using Improvement Maps in the operating theatre, it is possible to identify the region in the brain where electrical stimulation triggers the greatest improvement,” explains the researcher. “It can also help to avoid areas of the brain where stimulation causes adverse effects such as speech disorders.” Around 200,000 people worldwide have already been treated with deep brain stimulation, including in Switzerland. The procedure involves drilling a small hole in the skull and pushing a needle-thin test electrode down to the basal ganglia in the brain. There, the neuronal activity is measured: electrical signals originating from nerve cells, which are different for each brain region and thus facilitate orientation in the brain during surgery. When reaching the region of interest, it is stimulated several times with a very weak electrical current. The patient is awake during the procedure because the therapeutic effects cannot be observed under general anaesthesia. Some of the stimulation improvements can be seen immediately according to Hemm-Ode: “For example if the patient’s hand trembles at rest, when the stimulation begins the shaking decreases and ideally, is finally completely suppressed by the weak electrical stimuli.”
HLS researchers have developed a method to make deep brain stimulation in Parkinson’s disease even more precise and thus more effective. Deep brain stimulation, in which an electrode is implanted in the patient’s brain, is a treatment for the symptoms of tremor and rigidity. The positioning of the electrode in the brain affects the level of improvement in the symptoms. The HLS’s data-supported imaging method can identify the best stimulation location more reliably, enabling better intervention planning.
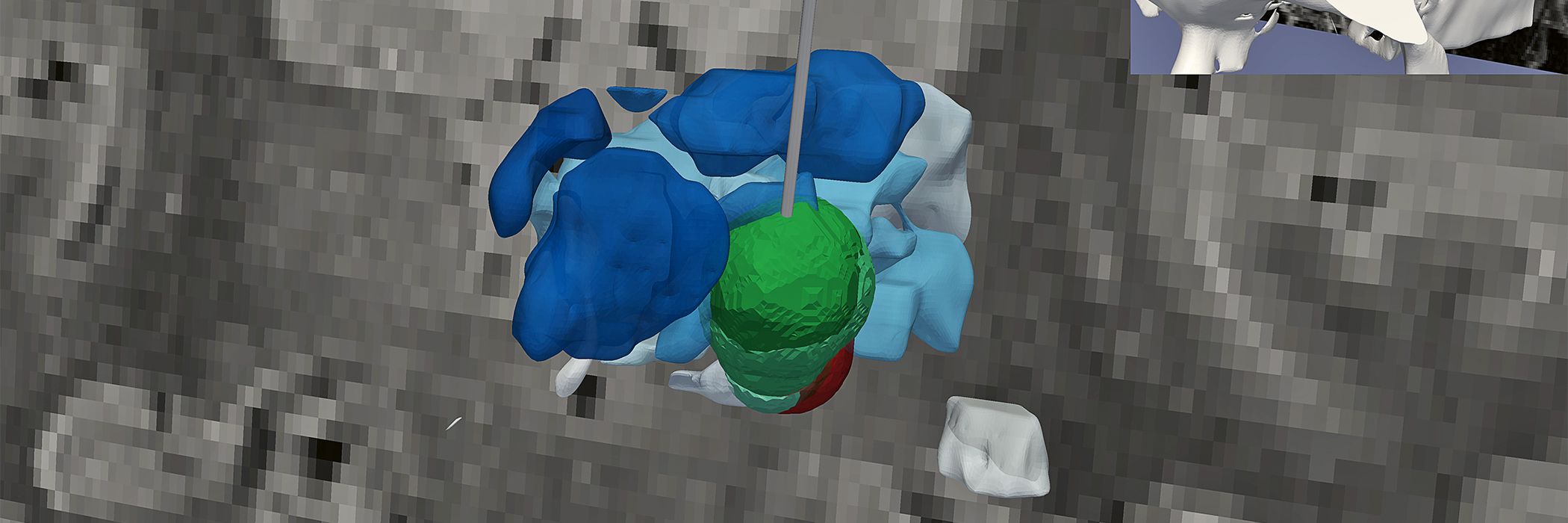
Until now, doctors wrote down information about stimulation during the operation: the location of the electrode in the brain, how deep it was inserted, the current used to stimulate the brain region, its effect on symptoms and any side effects. The Improvement Map makes all this information visible digitally on individual layered images taken from previous MRI scans. Brain structures such as the basal ganglia can be seen in shades of blue and there are a range of fields on a red/green colour scale. The darker the green, the greater the improvement in symptoms such as tremor, whereas red shows where adverse effects have occurred. The two areas can overlap. Acceleration sensors attached to the arm during the examination provide information on how severe the tremor or rigidity is.
“The aim is to use all this information to find the best possible point for long-term electrical stimulation,” explains Ashesh Shah, postdoctoral fellow at IM2. The smaller the brain area stimulated, the fewer the adverse effects. In addition, the electrical current required is lower, extending the battery life of the stimulator. Like a pacemaker, this battery is implanted under the skin and is connected to the electrode via a thin cable. Replacing it necessitates a small operation, hence extending battery life means less disruption for the patient.
The HLS researchers developed the Improvement Maps with a team from the University of Linköping in Sweden and the Clermont-Ferrand University Hospital in France, using clinical study data from patients with Essential Tremor or Parkinson’s disease. After the operation, they used this data to create 3D simulation models which, for each patient, show the precise location in the brain where stimulation brings the greatest improvement. The next step for the team is to make this visualisation available during surgery in real time.
- Intraoperative quantitative tremor and rigidity evaluation
- Acceleration sensor recording and analysis
- Surgical planning
- Patient-specific brain models of the thalamic region
- Patient-specific electric field simulations
- 3D data analysis
- 2D and 3D patient-specific data visualisationMethods
- Acceleration sensors
- Acceleration sensor platform for symptom evaluation
- 3D printed biocompatible sensor housing
- Data acquisition software
- Stereotactic frame
- X-ray systems
- Brainlab ‘iPlan’ surgical planning software and export tool
- Matlab for data analysis
- Paraview for visualisationInfrastructure
- Swiss National Science Foundation
- SATW Germaine de Staël Support
- University Hospital Basel
- University Hospital Bern
- University Hospital Clermont-Ferrand, FR
- Linköping University, SE Collaboration